Duetact
"Cheap duetact 17mg on line, diabetes type 1 is it genetic".
By: W. Jorn, M.B.A., M.B.B.S., M.H.S.
Clinical Director, Syracuse University
Here diabetes symptoms of purchase duetact once a day, a fallopian tube prolapse after hysterectomy created a conduit for peritoneal leakage of fluid diabetic low blood sugar purchase duetact amex. Immediate urinary leakage is suggestive of an unrecognized injury or failed repair of a recognized injury diabetes treatment victoza buy genuine duetact. Electrocautery-related injuries and ischemic trauma caused by clamps, sutures, or ureteral devascularization often have delayed presentations, typically 7–10 days after surgery [14]. Patients undergoing pelvic surgery in previously irradiated field can present weeks to years after their surgery [35,38]. Patients with ureterovaginal fistulas may not experience any urinary incontinence for 7–14 days after surgery, at which point a mucosa lined tract has had the opportunity to develop between the ureter and vagina [51]. These patients may, however, initially present with nonspecific symptoms such as low-grade fever, nausea, paralytic ileus, and flank pain, due to the developing urinoma and obstruction [5]. Although some vesicouterine fistulas present with both cyclical hematuria and vaginal urinary incontinence, other patients without urinary incontinence may not have any symptoms until they develop gross hematuria (menouria) during their menstrual cycle rather than the expected vaginal bleeding [40]. Physical Examination A thorough physical examination should be performed to evaluate for any signs or sequela of urogenital fistula. Prior to pelvic examination, a careful abdominal examination should be performed to evaluate for abdominal distension, tenderness, and flank pain. In all postsurgical patients, abdominal incisions should be inspected for signs of infection, drainage, or dehiscence. For a variety of reasons, patients often fail to provide accurate surgical histories. The physical examination is an excellent opportunity to review the abdominal and pelvic surgical history. The pelvic examination should assess for fluid in the vaginal canal, which can be collected and sent for creatinine levels [29]. The patient can also be asked to provide tampons or pads for creatinine evaluation. A urine specimen should be sent for urinalysis and culture to allow treatment of urinary tract infections prior to surgical repair. A careful speculum examination with appropriate lighting is needed to help identify and determine the size, character, number, and location of the fistula(s) (Figure 106. Special attention should be given to the vaginal cuff, anterior vaginal wall, and the cervical os. Irradiated patients may have friable lesions that present months and even years after their treatment. These lesions should be documented and subsequently biopsied to rule out the recurrence of malignancy [35,75]. However, smaller fistulas can be difficult to identify on physical exam and often require further investigation with examination under anesthesia, endoscopic evaluation, and imaging. If vaginal atrophy is present on exam, it should be treated preoperatively with topical vaginal estrogen to improve the quality of the vaginal epithelium to aid in surgical repair. Finally, the patient’s body habitus, genital 1567 anatomy, vaginal tissue quality, and the extent of tissue loss should be documented to aid in presurgical planning. A narrow introitus may warrant relaxing incisions at the time of repair to provide adequate access to the fistula [6]. Although the dye test is considered a routine diagnostic test for urogenital fistula, there are no large series to our knowledge that report the sensitivity or specificity of this test. The dye test is performed by filling the bladder with dilute methylene blue [77] or indigo carmine [39] solution (up to 300 mL). If the fistula is not seen, a tampon can be placed into the vagina, and the patient is asked to ambulate, and the vaginal packing is evaluated. If blue staining is noted, the pattern of staining can provide useful information about the possible location of the fistula. The blue dye test has been used in the literature to diagnose vesicouterine fistulas. Once the urine is noted to be orange, the bladder is emptied and filled with 300 mL of blue dye diluted in normal saline solution.
Other problems with both techniques include depression of automaticity blood sugar readings for diabetics generic 17mg duetact mastercard, pacemaker shifts diabetes mellitus rash order 16mg duetact overnight delivery, sinus entrance block diabetes diet not to eat order duetact 16 mg, and shortening of sinus action potential leasing to earlier onset of phase 4, each of which can give misleading results. We have found both techniques to give fairly comparable results in normal persons, particularly (but not necessarily) when cycle lengths of at least 50 msec less than sinus are used (Fig. A second method for circumventing sinus arrhythmia is the use of atrial 50 extrastimuli during atrial pacing. Analysis 41 55 of postreturn cycles (A3-A4) may provide insight into changes in automaticity or pacemaker shift. The coupling interval at which incomplete interpolation is first observed defines the refractory period of the perinodal tissue. In this instance, A3 represents delay of A1 exiting the sinus node, which has not been affected. The A1-A2 at which complete interpolation is observed probably defines the effective refractory period of the most peripheral of the perinodal tissue, because the sinus impulse does not encounter refractory tissue on its exit from the sinus node. In this instance, A1-A2 + A2-A3 = A1-A1, and sinus node entrance block is said to exist. Even after autonomic blockade, the range of “normals” reflects the previously described fallibility of the assumptions of indirect measurements as well as the variability of pacing site relative to the site of sinus impulse formation. B: The same patient is paced at a cycle length of 675 msec leading to a postdrive return cycle length of 805 msec followed by a sinus cycle length of 705 msec. Further work using endocardial recordings from the intact canine heart confirmed the ability to record diastolic phase 4 slope, followed by slow upstroke culminating in a 59 rapid atrial electrogram. Subsequently, several investigators developed techniques to record electrograms from 46 60 61 62 human subjects with and without sinus node dysfunction. Two techniques have been employed; in one the catheter is positioned at the junction of the superior vena cava and right atrium in the region of the sinus node, and the other – which appears more reliable and from which more stable recordings can be obtained – requires that the catheter be looped in the right atrium with firm contact at the region of the superior vena cava and atrial junction (Fig. This latter method, which produces firm contact against the atrial wall, produces an atrial injury potential simultaneously with the recording of the sinus node electrogram. The reported frequency for obtaining node electrograms ranges considerably, from 40% to 90%. Those studies using methods similar to the second method report higher success rates. In addition, filter settings play a prominent role in the ability to record stable electrograms that are not obscured by marked baseline drift. Use of low-end filter settings of 1 Hz or more produces diminution or loss of the sinus node electrogram. The high-end or low-pass filter frequency can be set at 20 or 50 Hz, the latter being more commonly employed. Using these techniques, which are time consuming, a stable sinus node electrogram without significant baseline shift can be recorded. However, in my opinion, the frequency and ease with which this recording can be made have been exaggerated. We obtained stable sinus node electrograms in only 50% of an unselected population of patients. It has been recognized that factors that produce encroachment of the T and U wave on the P wave make it P. If such patients are included in the unselected population of patients in whom sinus node electrogram requirements are attempted, the incidence of adequate recordings will be markedly diminished. Baseline drift is an important problem in preventing the recording of stable electrograms for measurements. Such drifts are more marked in young children and in those with significant cardiopulmonary disease and exaggerated respirations. Such baseline sinus drift can be obviated by using a low-end filter frequency of 0. There is an early return beat (A3), with an atrial activation sequence and P-wave morphology identical to that of sinus rhythm. Since the A1-A3 (650 msec) is less than the spontaneous sinus cycle length (790 msec), A3 is probably due to reentry in the region of the sinus node. On the right, a second method of obtaining the sinus node electrogram is shown with a catheter-looped positioning of the recording electrodes at the sinus node area. The human sinus node electrogram: a transvenous catheter technique and a comparison of directly measured and indirectly estimated sinoatrial conduction time in adults. When sinoatrial conduction is slowed, an increasing amount of the sinus node potential becomes visible before the rapid atrial deflection is inscribed.
Order duetact discount. TMS #498 - That Milford Show Medical - Diabetes Education.
Patients who easily desaturate with activity or who run lower than normal oxygen saturations at sea level will also require supplemental oxygen during fight blood glucose in dogs order duetact 16mg with amex. However diabetes symptoms juvenile order duetact with mastercard, the availability and cost of supplemental oxygen vary depending on the airline; even those airlines offering oxygen will usually only offer it during fight diabetes type 2 list of foods to eat discount duetact 17mg fast delivery. In addition, oxygen carried on the plane is primarily intended for use through emergency drop-down masks that are released only in the event of an in-fight emergency, such as decompression of the cabin. Travelers who require oxygen continuously from point of origin to destination are best advised to make individual arrangements for continuous supplemental oxy- gen using portable oxygen concentrators. Because 14 Prefight Therapies to Minimize Medical Risk Associated with Commercial Air Travel 143 in-seat electrical power is unavailable on the majority of aircraft, and even if avail- able is not guaranteed, passengers must travel with a supply of batteries that will have ample power for the full duration of the fight and all ground connections, in addition to unanticipated delays [3]. Passengers and their medical provider should consult with the air carrier in advance to determine whether a medical certifcate is required and whether details on the use of oxygen need to be specifed in advance. Strict instructions on the use of oxygen should include whether to be used for all or a portion of the fight, spe- cifc instructions on the maximum oxygen fow rate in liters per minute, a statement on the expected total operating time of the concentrator, and instructions to ensure that there is an adequate battery supply [3]. Patients with a stable ground-level PaO2 of greater than 70 mmHg, or a stable oxygen saturation of greater than 94%, should not require in-fight medical oxygen therapy. A practical ftness-to-fy test is to see if a patient can walk 50 yards at a normal pace or climb one fight of stairs without becoming severely short of breath. This test is performed by having the patient breathe an 85% nitrogen and 15% oxygen mixture, which is intended to simulate the aircraft cabin environment at altitude. Indicators of the need for in-fight supplemental oxy- gen include: PaO2 reduction to less than 55 mmHg and/or oxygen saturation reduc- tion to less than 85% [4]. Their ability to hyperventilate to compensate for hypoxemia is very limited, and clinicians should have a low threshold for recom- mending supplemental oxygen in these chronically-compromised patients. Patients with active or contagious tuberculosis are unsuitable for commercial air travel until there is documented improvement with treatment to control the infec- tion. For the safety of other passengers, patients with viral infection such as infu- enza should postpone air travel until clinically improved. Patients with bacterial pneumonia may travel when clinically stable, although they should be assessed for the advisability of supplemental oxygen during fight. Patients with a pneumothorax cannot travel by air due to the risk of the pneumothorax expanding during fight and possibly progressing to a tension pneumothorax. Patients who have had a pneumo- thorax successfully drained can travel once a normal chest radiograph has been obtained; the specifc waiting period for nonurgent commercial air travel is not known. Some stable patients with a pneumothorax may safely travel with a thora- cotomy catheter and a one-way Heimlich valve assembly [5]. Patients who have had uncomplicated thoracic surgery, or had drainage of the pleural effusion, should wait 1–2 weeks before traveling and be assessed for the re-accumulation of fuid and/or the presence of a pneumothorax prior to departure. Patients with interstitial lung disease, malignancy, cystic fbrosis, neuromuscular disease, and pulmonary hyper- tension should be assessed for the need for in-fight medical oxygen. However, the following are frequently suggested by experts and guideline committees for passengers during extended travel of 6 h or greater: fre- quent ambulation, every 1–2 h, frequent fexion and extension of the ankles and knees, and avoidance of agents that may promote immobility or dehydration, such as drugs and alcohol. Based on limited data, it would be reasonable to recommend that low- risk patients be advised to maintain hydration and avoid immobility, and that moderate-risk patients add compression stockings to the low-risk recommenda- tions. Passengers compensate for in-fight hypoxia by increasing minute ventilation, and most develop a mild tachy- cardia which increases myocardial oxygen demand. This increased heart rate may cause patients with cardiac disease to decompensate. Patient should be cautioned to carry their medications on board with them and to take them at prescribed intervals. One retrospective study examined the incidence of in-fight adverse events among patients who were returning home after treatment for unstable angina pectoris or acute myocardial infarction. Patients with uncomplicated percutane- ous coronary interventions are at low risk for travel by commercial airline once they remain stable and have resumed normal activities. Cardiac surgery, including coronary artery bypass grafting, poses no intrinsic risk to passengers aboard aircraft. These patients should be assessed for the risk of barotrauma due to decreased atmospheric pressure and should be assessed for the possibility of pneumothorax or pneumopericardium prior to travel [5]. Pacemakers and implantable defbrillators pose a low risk for travel by commercial airline once the patient has been deemed to be medically stable.
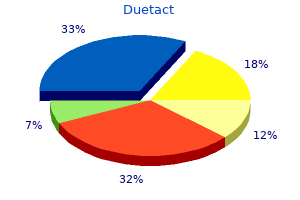
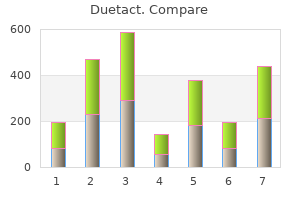
Three studies indicated that symptomatic women had slower urine flow rates than normal women with one study [15] showing no difference blood sugar and blood pressure buy 16mg duetact. The flow data for these women were converted to centiles from the Liverpool Nomograms for the following analyses of their median values: A Comparison of the Urine Flow Rates of Symptomatic and Asymptomatic Women Table 53 diabetes testing kit reviews order duetact in india. There was a close agreement between the studies with the 1990 study [30] performed in a different country to the 1995 study [31] diabetes mellitus fact sheet order online duetact. Effect of the Presence of Genital Prolapse on Urine Flow Rates in Symptomatic Women A generally progressive decline in the maximum and average urine flow rates (median centiles) of symptomatic women [31] with increasing grades of genital prolapse was noted. The most significant decline occurred in the presence of uterine prolapse closely followed by cystocoele and enterocoele. More recent data [32], however, would suggest the significance of this may be lost in multivariate analysis of a much larger cohort of symptomatic women. The flow rates for those symptomatic women without prior hysterectomy was found to be the same as that for the asymptomatic female population. Further analysis suggests that in women with both prior hysterectomy and intercurrent genital prolapse, there is a cumulative decline in urine flow. More recent data [32], however, would suggest the significance of this may be lost in multivariate analysis of a much larger cohort of symptomatic women. Effect of Age and Parity on Urine Flow Rates in Symptomatic Women Unlike asymptomatic women, there is a significant effect of age on the maximum and average urine flow rates [30,31]. More recent data [32] suggest that age is the main association of abnormally slow urine flow rates in a large cohort of symptomatic women. Parity was not found to be a significant factor in either this or the 1999 study [31]. Effect of Final Urodynamic Diagnosis on the Urine Flow Rates of Symptomatic Women Median urine flow rate centiles of the urogynecology patients separated according to the final urodynamic diagnosis are given in Table 53. All categories of diagnoses have their median centiles under those for the normal female population (50 by definition). The situation during voiding is the antithesis of the situation required for continence. Continence depends on intraurethral pressure being higher than intravesical pressure. Einhorning [33] and later Asmusen and Ulmsten [34] showed clearly that before any rise in intravesical pressure, a fall in intraurethral pressure occurred. This suggests that the urethra actively relaxes during voiding rather than being passively “blown open” by the detrusor contraction. Soon after the urethra has relaxed and pelvic floor descent has occurred, the detrusor contracts. The detrusor normally contrives to contract until the bladder is empty, producing a continuous flow curve. Many women void by urethral relaxation alone with minimal or no detrusor involvement. Some women appear to void entirely 841 by increasing intra-abdominal pressure, that is, by contraction of the diaphragm and anterior abdominal wall muscles. It follows from this discussion that the urine flow may differ from normal as a result of abnormalities of the urethra or the detrusor. Urethral Factors Anatomical factors The urethra may be abnormally narrow or the urethra may not be straight. The narrowest part of the urethra, as shown by video studies of voiding, is usually the midzone. However, the urethra may become narrowed and the most common site is at the external meatus associated with estrogen deficiency in the postmenopausal women. Bladder neck obstruction in the female had been thought to be extremely rare [35]. The female urethra is usually straight, and deviation from this state is most common in anterior vaginal wall prolapse and higher degrees of uterine and vaginal vault prolapse.