Probalan
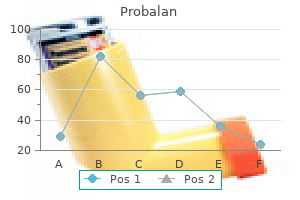
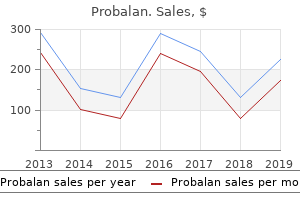
"Cheap 500mg probalan free shipping, treatment 2".
By: L. Ur-Gosh, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Deputy Director, University of Oklahoma School of Community Medicine
Content includes tools to identify and manage problem drinking ombrello glass treatment probalan 500 mg overnight delivery, plus a calculator for determining the alcohol content of various beverages symptoms rheumatic fever buy cheap probalan 500mg. Drugs for Alcohol Use Disorder In the United States about 1 million alcoholics seek treatment every year treatment 1 degree burn buy generic probalan on-line. Although the success rate is discouraging—nearly 50% relapse during the first few months—treatment should nonetheless be tried. Drugs Used to Treat the Symptoms of Withdrawal Management of withdrawal depends on the degree of dependence. When dependence is mild, withdrawal can be accomplished on an outpatient basis without drugs. The goals of management are to minimize symptoms of withdrawal, prevent seizures and delirium tremens, and facilitate transition to a program for maintaining abstinence. The benefits of benzodiazepines and other drugs used during withdrawal are shown in Table 31. In patients with severe alcohol dependence, benzodiazepines can stabilize vital signs, reduce symptom intensity, and decrease the risk for seizures and delirium tremens. Although all benzodiazepines are effective, agents with longer half-lives are generally preferred because they provide the greatest protection against seizures and breakthrough symptoms. The benzodiazepines employed most often are chlordiazepoxide [Librium, others], clorazepate [Tranxene], oxazepam (generic only), and lorazepam [Ativan]. Traditionally, benzodiazepines have been administered around-the-clock on a fixed schedule. Adjuncts to Benzodiazepines Combining a benzodiazepine with another drug may improve withdrawal outcome. Agents that have been tried include carbamazepine (an antiepileptic drug), clonidine (an alpha -adrenergic agonist), and atenolol and propranolol2 (beta-adrenergic blockers). Clonidine and the beta blockers reduce the autonomic component of withdrawal symptoms. It should be stressed, however, that these drugs are not very effective as monotherapy. Hence they should be viewed only as adjuncts to benzodiazepines—not as substitutes. Drugs Used to Maintain Abstinence After detoxification has been accomplished, the goal is to prevent—or at least minimize—future drinking. However, if drinking must resume, keeping it to a minimum is still beneficial because doing so will reduce alcohol-related morbidity. In trials of drugs used to maintain abstinence, several parameters are used to measure efficacy. These include the following: • Proportion of patients who maintain complete abstinence • Days to relapse • Number of drinking days • Number of drinks per drinking day In the United States only three drugs—disulfiram, naltrexone, and acamprosate—are approved for maintaining abstinence. Disulfiram Aversion Therapy Therapeutic Effects Disulfiram [Antabuse] helps alcoholics avoid drinking by causing unpleasant effects if alcohol is ingested. In clinical trials, there is emerging evidence that the drug may be only slightly better than placebo at maintaining long-term abstinence; however, long- term studies have not been completed. Disulfiram does decrease the frequency of drinking after relapse has occurred—presumably because of the unpleasant reaction that the patient is now familiar with. Supervised administration of disulfiram may be more effective than when patients self-administer the drug. Mechanism of Action Disulfiram disrupts alcohol metabolism by causing irreversible inhibition of aldehyde dehydrogenase, the enzyme that converts acetaldehyde to acetic acid. As a result, if alcohol is ingested, acetaldehyde will accumulate to toxic levels, producing unpleasant and potentially harmful effects. Pharmacologic Effects The constellation of effects caused by alcohol plus disulfiram is referred to as the acetaldehyde syndrome, a potentially dangerous event. In its “mild” form, the syndrome manifests as nausea, copious vomiting, flushing, palpitations, headache, sweating, thirst, chest pain, weakness, blurred vision, and hypotension; blood pressure may ultimately decline to shock levels. This reaction, which may last from 30 minutes to several hours, can be brought on by consuming as little as 7 mL of alcohol.
Intermittent inspiratory chest tube occlusion This synchronizes chest tube occlusion on inspiration medicine 751 buy 500mg probalan overnight delivery, potentially reducing the leak and facilitating distribution of tidal volume to the rest of the lung symptoms 9 weeks pregnant cheap probalan 500mg with amex. The underwater seal is connected to the inspiratory limb of the ventila- tory circuit through a pressure-amplifying valve treatment dynamics order 500mg probalan with visa. The positive pressure gen- erated on inspiration closes the outlet of the underwater seal and thereby the chest tube. Also, many of these patients are too ill to risk surgical repair, and non- surgical methods need to be considered. Pleurodesis In chemical pleurodesis, a sclerosant is instilled through the chest tube when the lung is fully re-expanded. However, the chest tube needs to be clamped after instillation of the sclerosant (contraindicated in the pres- ence of an air leak). One way around this is to elevate the connecting tube between the chest tube and the underwater seal up to 60cm above 5. Raising the tubing (but not the bottle containing the underwater seal) prevents the sclerosant immediately trickling out of the chest drain but still allows air to escape. Because of the relatively high failure rates (in the region of 10%) with pleurodesis compared with surgical pleural stripping procedures, pleurodesis is usually only consid- ered for those patients who are either unwilling or too unwell to undergo surgery. Pleurectomy This involves stripping the parietal pleura to encourage the lung to stick to the chest wall in an attempt to obliterate the pleural space and achieve symphysis. The pleurectomy may be total or partial (where the medi- astinal and diaphragmatic pleural surfaces are just abraded rather than stripped) and it can be performed thoracoscopically or via open thora- cotomy. Video-assisted thoracoscopic pleurectomy has been shown to be a successful intervention with a relatively low risk of complication (recur- rence, bleeding, chronic chest wall pain) in patients with recurrent primary spontaneous pneumothoraces (a pneumothorax arising in an otherwise healthy person without any lung disease). However, open thoracotomy is still recommended in patients with secondary pneumothoraces (sec- ondary to underlying lung disease), which would include most critically ill patients with a pneumothorax. Pleurectomy is usually performed under general anaesthesia with one-lung ventilation and unfortunately many crit- ically ill patients are too sick to tolerate this. Endoscopic repair If the leak can be identified it may be amenable to endoscopic or endo- bronchial closure. None of these methods have been subjected to rigorous, systematic clin- ical evaluation and the decision to use any one of them is usually based on local experience and expertise. The diagnostic approach and diagnostic criteria are not standardized and at least six different diagnostic methods have been described: • Quantitative and qualitative cultures of tracheal aspirates • Bronchial brushings with and without bronchoscopy • Bronchoalveolar lavage with and without a bronchoscopy. Such diagnostic uncertainty leads to lack of consensus on basic information such as incidence (quoted incidence ranges from 9% to 28%), treatment, and outcome. In illness, this flora is replaced by pathogenic organisms, most notably enteric aerobic Gram- negative bacilli and Staphylococcus aureus. This change in microbial flora is directly related to the severity of illness of the patient, rather than environmental factors (healthy individuals who work in hospitals do not become colonized) or antibiotic use (it occurs in patients who have not received antibiotics). Bacteria may gain access to the lower respiratory tract either at or following intubation. The inner surface of the tracheal tube also acts as a nidus for biofilm formation, which protects the colonizing pathogens. Ventilator cycling and the frequent passage of suction catheters through these tubes introduce the pathogens into the lower airway. Diagnosis The diagnosis of pneumonia in ventilated patients using clinical and radio- logical criteria alone is difficult. Microscopic analysis of tracheal aspirates is unreliable in predicting culture results and should not be used to guide antibiotic therapy. The presence of macrophages indicates that the specimen is from the lower respiratory tract. As neutrophils comprise up to 20% of the cells recovered from a routine mouthwash, they must be present in abundance on microscopy in order to be used as evidence of infection. A gelatine plug seals the sampling brush in the inner lumen of a catheter, preventing upper airway contamination. Catheters are usually placed by brochoscopic control, although blind sampling devices are now available (protected catheter specimen). Antibiotic guidelines A variety of factors should influence the choice of initial antibiotic therapy, including knowledge of the likely organisms and their sensitivities, local microbial epidemiology, and the results of surveillance cultures from the patient.
In many patients symptoms retinal detachment order probalan 500mg line, side effects can be reduced simply by decreasing the dosage (typically by 25%) symptoms xylene poisoning purchase probalan online now. If dosage reduction causes pain to return symptoms zoloft overdose purchase generic probalan from india, adding a nonopioid analgesic may take care of the problem. Over time, tolerance develops to sedation, respiratory depression, nausea, and vomiting—but not to constipation or miosis. Respiratory Depression Respiratory depression is the most serious side effect of the opioids; death can result. Fortunately, when dosage and monitoring are appropriate, significant respiratory depression is rare. Respiratory depression is greatest at the outset of treatment and then decreases as tolerance develops. Significant respiratory depression is most likely when dosage is being titrated up. The best way to assess the risk for impending respiratory depression is to monitor opioid-induced sedation. An increase in sedation generally precedes an increase in respiratory depression, so if excessive sedation is observed, further dosing should be delayed. Severe respiratory depression can be reversed with naloxone [Narcan], a pure opioid antagonist. However, caution is required: excessive dosing will reverse analgesia, thereby putting the patient in great pain. When death is near, should opioids be withheld out of fear that respiratory depression may bring death sooner? Third, when death is imminent, it is more important to provide comfort than prolong life. Accordingly, adequate opioids should be provided, even if doing so means life ends a bit sooner. Opioids promote constipation by decreasing propulsive intestinal contractions, increasing nonpropulsive contractions, increasing the tone of the anal sphincter, and reducing fluid secretion into the intestinal lumen. For prophylaxis of constipation, current guidelines recommend daily therapy with a combination product, such as Senokot-S, which contains both senna and docusate. Methylnaltrexone [Relistor] is indicated only for constipation in patients with end-stage disease. If sedation persists, it can be reduced by giving smaller doses of the opioid more frequently, while keeping the total daily dose the same. Other Side Effects Opioids promote histamine release and can thereby cause itching, which can be relieved with an antihistamine (e. Opioids increase the tone in the urinary bladder sphincter and can thereby cause urinary retention. Benign prostatic hypertrophy and use of anticholinergic drugs will exacerbate the problem. Patients should be monitored for urinary retention and encouraged to void every 4 hours. Patients should be informed about symptoms of hypotension (lightheadedness, dizziness) and instructed to sit or lie down if they occur. Orthostatic hypotension can be minimized by moving slowly when changing from a supine or seated position to an upright posture. Primary risk factors are renal impairment, preexisting cognitive impairment, and prolonged, high- dose opioid use. Adjuvant Analgesics Adjuvant analgesics are used to complement the effects of opioids. Accordingly, these drugs are employed in combination with opioids—not as substitutes. Adjuvant analgesics can (1) enhance analgesia from opioids, (2) help manage concurrent symptoms that exacerbate pain, and (3) treat side effects caused by opioids. The adjuvant analgesics differ from opioids in that pain relief is limited and less predictable and often develops slowly. The adjuvants are interesting in that, although they can relieve pain, all of them were developed to treat other conditions (e.
Purchase probalan. The benefits of quitting smoking.
Syndromes
- Anti-glomerular basement membrane antibody
- Heart murmurs
- Peeling skin
- Medicines applied to the skin including corticosteroids, immunotherapy, and minoxidil
- Blood culture
- Colonoscopy
- Age 7-12 months: 6* mcg/day
- Avoid eating heavy meals at least 2 hours before going to sleep.
As noted previously medicine 7767 cheap probalan online, overdose with a cholinesterase inhibitor can produce cholinergic crisis medicine 54 357 buy probalan 500mg visa. Like myasthenic crisis medications given im purchase probalan australia, cholinergic crisis is characterized by extreme muscle weakness or frank paralysis. In addition, cholinergic crisis is accompanied by signs of excessive muscarinic stimulation. The offending cholinesterase inhibitor should be withheld until muscle strength has returned. Because myasthenic crisis and cholinergic crisis share similar symptoms (muscle weakness or paralysis), but are treated very differently, it is essential to distinguish between them. A history of medication use or signs of excessive muscarinic stimulation are usually sufficient to permit a differential diagnosis. If these clues are inadequate, the provider may elect to administer a challenging dose of edrophonium, an ultrashort-acting cholinesterase inhibitor. If edrophonium-induced elevation of acetylcholine levels alleviates symptoms, the crisis is myasthenic. Because the symptoms of cholinergic crisis will be made even worse by edrophonium and could be life-threatening, atropine and oxygen should be immediately available whenever edrophonium is used for this test. Toxicology of Muscarinic Agonists Sources of Muscarinic Poisoning Muscarinic poisoning can result from ingestion of certain mushrooms (e. Symptoms Manifestations of muscarinic poisoning result from excessive activation of muscarinic receptors. Prominent symptoms are (1) respiratory (bronchospasm and excessive bronchial secretions); (2) cardiovascular (bradycardia and hypotension); (3) gastrointestinal (profuse salivation, nausea and vomiting, abdominal pain, diarrhea, and fecal incontinence); (4) genitourinary (excessive urination and urinary incontinence); integumentary (diaphoresis); and visual (lacrimation and miosis). Some common mnemonics can help you to identify this potentially dangerous condition. Mnemonic 1: Dumbels Diaphoresis/Diarrhea Urination Miosis Bradycardia/Bronchospasm/Bronchorrhea Emesis Lacrimation Salivation Mnemonic 2: Sludge and the Killer Bs Salivation Lacrimation Urination Diaphoresis/Diarrhea Gastrointestinal cramping Emesis Bradycardia Bronchospasm Bronchorrhea Treatment Management is direct and specific: administer atropine (a selective muscarinic blocking agent) and provide supportive therapy. By blocking access of muscarinic agonists to their receptors, atropine can reverse most signs of toxicity. Muscarinic Antagonists (Anticholinergic Drugs) Muscarinic antagonists competitively block the actions of acetylcholine at muscarinic receptors. Because most muscarinic receptors are located on structures innervated by parasympathetic nerves, the muscarinic antagonists are also known as parasympatholytic drugs. Additional names for these agents are antimuscarinic drugs, muscarinic blockers, and anticholinergic drugs. This term is unfortunate in that it implies blockade at all cholinergic receptors. However, as normally used, the term anticholinergic only denotes blockade of muscarinic receptors. Therefore, when a drug is characterized as being anticholinergic, you can take this to mean that it produces selective muscarinic blockade—and not blockade of all cholinergic receptors. In this chapter, the terms muscarinic antagonist and anticholinergic agent are used interchangeably. Atropine Atropine [AtroPen, others] is the best-known muscarinic antagonist and will serve as our prototype for the group. Mechanism of Action Atropine produces its effects through competitive blockade at muscarinic receptors. Rather, all responses to atropine result from preventing receptor activation by endogenous acetylcholine (or by drugs that act as muscarinic agonists). At therapeutic doses, atropine produces selective blockade of muscarinic cholinergic receptors. However, if the dosage is sufficiently high, the drug will produce some blockade of nicotinic receptors, too. Pharmacologic Effects Because atropine acts by causing muscarinic receptor blockade, its effects are opposite to those caused by muscarinic activation. Accordingly, we can readily predict the effects of atropine by knowing the normal responses to muscarinic receptor activation (see Table 11.