Effexor XR
"Order 75mg effexor xr with visa, anxiety symptoms 9 dpo".
By: W. Fadi, M.A.S., M.D.
Clinical Director, Roseman University of Health Sciences
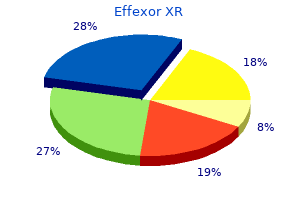
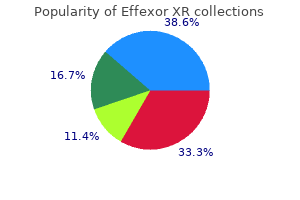
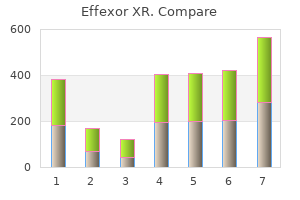
Compassionate and palliative care Palliative care after birth may be the preferred option for Resuscitation plan for high‐risk deliveries some babies anxiety symptoms tinnitus buy effexor xr 150 mg. There is increasing awareness of the need Formal resuscitation plans are required for certain high‐ for palliation anxiety symptoms anxiety attacks cheap effexor xr online mastercard, improving management and increasing risk deliveries anxiety journal template buy effexor xr 150mg on-line, such as extreme prematurity at the mar- availability of resources for neonatal palliative care. Neonatal Care for Obstetricians 447 Communication following neonatal death Neonatal transport In circumstances where neonatal death is the outcome, Ensuring that babies receive the appropriate level of care family support by neonatal staff should include the ante- ideally requires delivery in the correct place if delivery natal team wherever possible. Continuing engagement is predictable and safe antenatal transfer of mother is by the obstetric staff in the postnatal care of the baby possible. Postnatal transfer of babies to the correct level and family is especially helpful when the outcome is of unit after delivery also needs to be available. This ongoing com- neonatal transfer services are evolving that have the munication between the antenatal and postnatal teams expertise and equipment and thus help to avoid deplet- improves quality of care for the individual family and for ing specialist staff from the either the referral unit or the all babies in general, as open dialogue fosters respect specialist centre. In order to facilitate family involve- ment, it is also expected that the infant should be cared Providing the appropriate level of care for the mother for within the network rather than being transferred and/or her baby requires careful planning and well‐ great distances. Managed neonatal clinical networks Birth and postnatal adaptation: neonatal resuscitation Managed health service networks aim to deliver appro- priate healthcare to a defined local population in the Only 1% of normal birthweight babies require active most effective and efficient manner. Although the need for resuscitation may be Department of Health Toolkit for High‐Quality Neonatal predictable based on risk factors, 30% of babies requiring Services [6] set the standards of care that should be pro- resuscitation are not predicted. Included in these rec- risk of not making a successful adaptation without assis- ommendations was the stipulation that neonatal care tance include those in the following groups: preterm should be delivered in managed clinical networks. The level of meconium‐stained liquor, malpresentation and breech, care provided by each hospital is based on resources, multiple pregnancies, caesarean section under general capacity, geography and the availability of appropri- anaesthesia or for fetal distress, risk of fetal infection and ately skilled and trained staff. The development of coterminous maternity net- that all professionals present at the time of birth are pro- works are also enhancing the organization of perinatal ficient in resuscitation of the newborn [7]. These units have 24‐hour cover from specialized nursing staff and neona- tal specialist doctors. Local neonatal (level 2) units pro- Antenatal and newborn screening vide respiratory support for babies of 28 weeks’ gestation or more and special care (level 1) units provide care Antenatal screening continues after birth with newborn for babies that do not require respiratory support for screening programmes. In England and Wales, there were 700 000 liveborn babies in 2013, 7% preterm and 1. England Wales Scotland Ireland the infant mortality rate (deaths at less than 1 year of age) in term infants was 3. Of those born at less than 32 Cystic fibrosis √ √ √ √ weeks of gestation, 15% resulted in an infant death and this Sickle cell disease √ √ √ √ accounted for over half of all infant deaths. Variation may Phenylketonuria √ √ √ √ be due to methodological differences such as case ascer- Medium‐chain acyl √ √ √ √ tainment, selection bias, and varying outcome definitions dehydrogenase deficiency and follow‐up duration. Reports from geographically Maple syrup urine disease √ √ – – defined population‐based studies show lower survival rates than single‐centre selective studies that are subject to bias. Isovaleric acidaemia √ √ – – Variation in preterm birth rates (all births) also appears Glutaric aciduria type 1 √ √ – – to have a major influence on reported neonatal mortal- Homocystinuria √ √ – – ity rates between populations. European regions, the delivery rate per 1000 births +6 between 22 and 31 weeks in two regions in England (Trent: 16. Live birth influence antenatal management of mother and fetus rates showed similar trends. When comparisons were and, in some cases, postnatal management of the made between regions after adjustment for prematurity newborn. The specific and whether neonatologists perform resuscitation and areas included are the detection of congenital cata- redirection of care during intensive care, all potentially racts (red reflex), congenital heart disease, develop- have effects on reported survival and outcome. There are limited data on longer‐term morbidity in this group but recent reports suggest this neglected area should be Neonatal outcome studied in greater detail. There are five times more late preterm babies born than babies born before 32 weeks’ Prematurity gestation and therefore as a group require considerable Prematurity is the major determinant of neonatal out- healthcare resources. Overall rates do not appear to be changing signifi- the following two decades, the use of antenatal corticos- cantly as survival increases, but there is concern that the teroids, use of surfactant and improvements in respira- absolute prevalence will increase with increased survival tory support have resulted in striking improvements in of the most immature babies. During the study regionalized neonatal care was percentage of those with developmental impairment poorly developed.
Additional information:
Arterial blood gas usually reflects hypoventilation acute anxiety 5 letters generic effexor xr 75mg, respiratory acidosis 0800 anxiety buy cheap effexor xr 150mg on line, and metabolic acidosis [40] anxiety gif buy effexor xr 37.5mg amex. If pulmonary edema develops, chest radiographs typically reveal bilateral fluffy alveolar infiltrates, occasionally unilateral in nature, and echocardiograms show normal cardiac function [41]. A negative anion gap with hyperchloremia should raise the suspicion of bromide poisoning from chronic dextromethorphan use, and can be confirmed by a serum bromide level [12]. Leukoencephalopathy associated with inhalational abuse of heroin appears as hypoattenuation in the affected white matter, although this may not be apparent until late in the disease. Magnetic resonance imaging typically demonstrates white matter hyperintensity on T2- weighted sequences. The affected areas are initially the occipital and cerebellar white matter, followed by involvement of the parietal, temporal, and frontal lobes. The cerebellar peduncles, splenium of the corpus callosum, posterior limb of the internal capsules, corticospinal tract, medial lemniscus, and tractus solitarius may also be involved [23]. A urine toxicology screen may confirm the diagnosis, but is rarely necessary for acute patient management. The metabolites of naloxone are chemically related to oxymorphone, but naloxone is not known to give false-positive immunoassay urine screens for opioid substances [43]. However, the classic triad of opiate toxicity (coma, miosis, and respiratory depression) may not be apparent after a mixed overdose. Respiratory support is paramount in the management of patients with opioid toxicity; one should secure the airway and ventilate with 100% oxygen. Repeat naloxone boluses may be required every 20 to 60 minutes because of its short elimination half-life (60 to 90 minutes). A continuous naloxone infusion may be considered for patients who have a positive response but require repeated bolus doses because of recurrent respiratory depression [50]. A therapeutic continuous naloxone infusion can be made by administering two third of the effective naloxone bolus dose per hour (see Chapter 125-Antidotes). The infusion is titrated to maintain adequate spontaneous ventilation without precipitating acute opioid withdrawal and empirically continued for 12 to 24 hours. The patient should be admitted to an intensive care or high-dependency setting for continuous monitoring. After the naloxone therapy is discontinued, the patient should be carefully observed for 4 hours for recurrent respiratory depression. Nebulized naloxone, 2 mg mixed with 3 mL normal saline delivered by a nebulizer face mask with the side ports partially occluded with tape to prevent excessive loss of medication, appears to be a safe and effective treatment of suspected opioid overdose in patients with a minimum respiratory rate of 6 breaths per minute [51]. All patients with significant diphenoxylate overdose should be observed in an intensive care setting for at least 24 hours. The management of seizures should follow current treatment guidelines and include benzodiazepines or barbiturates. Adjunct naloxone therapy may be effective in propoxyphene, but not in meperidine- or tramadol-related seizures [52]. The clinical benefits of multiple oral doses of activated charcoal are unproven, but it is potentially beneficial because of the prolonged absorption phase that is typically encountered with opiate overdoses. The management of pulmonary edema should include adequate ventilation, oxygenation, and low tidal volume positive-pressure ventilation as needed [54]. Bradycardia secondary to methadone administration responds to ceasing the drug; atropine has not been utilized. Asymptomatic body packers should be conservatively managed when the condition of packaging does not appear to be compromised. One proposed guideline involves the oral administration of a water-soluble contrast solution followed by serial abdominal radiographs (Table 119. If radiographs are positive, perform daily abdominal radiographs, and after a spontaneous bowel movement 4. The patient may be discharged after passage of two packet-free bowel movements and negative abdominal radiographs a the patients are permitted to feed normally, and vascular access should be maintained. If there is an incomplete response or no response, additional doses can be given at 2- to 5-minute intervals. Anton B, Salazar A, Flores A, et al: Vaccines against morphine/heroin and its use as effective medication for preventing relapse to opiate addictive behaviors. Hagel J, Andrews G, Vertinsky T, et al: “Chasing the dragon”—imaging of heroin inhalation leukoencephalopathy. Sloth Madsen P, Strom J, Reiz S, et al: Acute propoxyphene self- poisoning in 222 consecutive patients.
As filtrate passes through the loop of Henle anxiety symptoms skin effexor xr 37.5 mg amex, solute is removed by the Na/K/2Cl transporter located in the cells of thick ascending limb and by the NaCl carrier in the distal tubule anxiety disorder test buy generic effexor xr 37.5 mg on-line. Solute entering the early proximal tubule has an osmolality identical to that of plasma; fluid is isotonically reabsorbed in this nephron segment anxiety symptoms 7 months after quitting smoking purchase effexor xr online. Separation of solute from water (H2O) within the tubule begins in the thick ascending limb of Henle, which is impermeable to H2O. For example, for a patient unable to achieve urinary dilution below an osmolality of 300 mOsm per kg, the amount of water that can be excreted on a normal diet is reduced to 3 L: 900 mOsm/300 mOsm/kg = 3 L As discussed earlier, solute excretion is normally determined by dietary intake. A reduction in dietary sodium and protein intake, as is seen in the patient on a “tea-and-toast” diet, limits the capacity to excrete water. If solute intake falls to 150 mOsm per day, for instance, water excretion is limited to approximately 3 L even when urinary dilution is normal: 150 mOsm/50 mOsm/kg = 3 L It is easy to see that the combination of impaired diluting ability with a concomitant reduction in solute intake is more likely to impair water excretion and result in hyponatremia than either disturbance alone. Hyponatremia In most settings, the development of hyponatremia with hypoosmolality represents the retention of ingested or administered water. Thus, the causes of hyponatremia can be divided into those in which water excretion is abnormal and those in which water excretion is normal, but water ingestion is considerably increased. An exception to this rule occurs when solute intake is markedly reduced, as in the patient subsisting on a solute-poor diet. Solute excretion tends to be reduced in these settings, which are characterized by enhanced tubular salt reabsorption. The ability to excrete dilute urine is impaired by diuretics, whether they act in the thick ascending limb of Henle (loop diuretics) or in the distal tubule (thiazide diuretics). Loop diuretics inhibit the Na-K-2Cl cotransporter in the medullary portion of the thick ascending limb of Henle, whereas thiazides block a simple NaCl carrier in the cortical portion of the distal tubule. These differences explain, in part, the susceptibility of individuals treated with thiazide-type diuretics to the development of hyponatremia (see text for details). This observation is attributable, in part, to different sites of the action within the renal tubule. Loop diuretics, which act in the outer medulla, reduce the solute concentration in the renal medullary interstitium. By comparison, thiazide diuretics, which act in the cortex, impair diluting capacity but have a lesser effect on concentrating ability. For reasons that are not well understood, however, most individuals with thiazide-induced hyponatremia gain weight, indicating that the hyponatremia is at least in part a result of increased water intake. This disorder occurs more frequently in women, typically occurs early in therapy (within 1 to 4 weeks), and is more likely to be observed in elderly individuals [3]. It is important to note that adrenocortical dysfunction (as in Addison’s disease) leads to reduced cortisol and aldosterone levels, the latter predisposing to hyperkalemia. The presence of a low cortisol level alone, because of either pituitary or hypothalamic disease, or the abrupt withdrawal from prolonged exogenous corticosteroid administration may cause hyponatremia but should not alter potassium homeostasis, because aldosterone release is normal. This disorder has been described in patients with hypovolemia, psychosis, and chronic malnutrition, as + well as in normal pregnancy (in which the plasma Na concentration decreases by the second trimester from 140 to 135 mEq per L). The diagnosis can be confirmed clinically by observing the response to a water load (10 to 15 mL per kg given orally or intravenously during 30 minutes). Mineralocorticoid replacement therapy with fludrocortisone acetate has been effective in some patients. As discussed previously, a reduction in salt and protein intake can lead to hypoosmolality if water intake exceeds output. Severely reduced solute intake, as occurs with a “tea-and-toast diet,” can cause hyponatremia even with normal degrees of water intake. The absence of polyuria and the development of hyponatremia with normal or slightly above normal fluid intake distinguish these individuals from those with primary polydipsia. Psychiatric patients, particularly those with schizophrenia, often have abnormalities in water balance. Depending on the abnormality that is present, the patient may present with polydipsia and polyuria or hyponatremia.